
Colorectal Cancer FACTS
 CRC as the third most common cancer and the second most common cause of death from cancer for both men and women.
CRC as the third most common cancer and the second most common cause of death from cancer for both men and women.
Yet CRC is a highly treatable cancer if it is detected early and it is up to 95 per cent preventable with timely and thorough testing or "CRC screening". Unfortunately as it stands today, nearly half of those diagnosed find out too late.
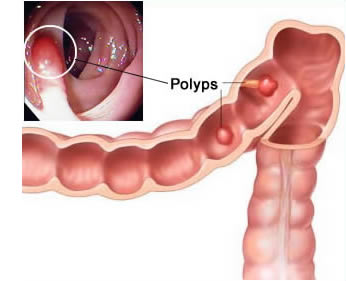
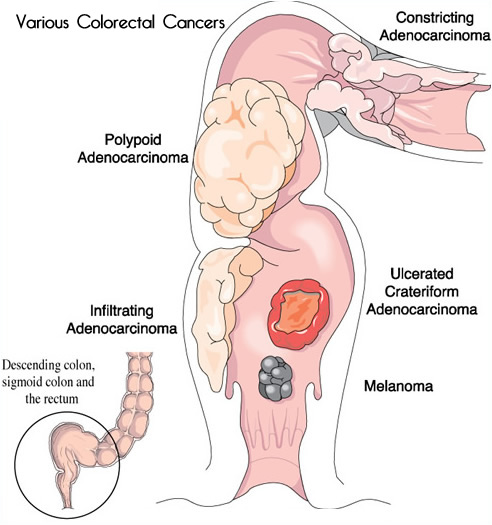
The majority of CRCs begin as benign growths in the lining of the colon called adenomatous polyps. Over the years, these polyps grow in size and number, thereby increasing the risk that the cells in the polyps will become cancerous. Timely removal of these growths - easily done during a colonoscopy - will prevent CRC from developing. It is important to identify and remove these polyps as soon as possible.
Polyp removal is usually done during a colonoscopy and the patient is sedated during the procedure. Recovery is very quick and usually pain-free. Polyps are sent for a biopsy and tested for any malignancies.
Colorectal Cancer by the Numbers:
- One in 14 men is expected to develop CRC during his lifetime and one in 27 will die of it.
- One in 15 women is expected to develop CRC during her lifetime and one in 31 will die of it.
- Anyone 50 and up should be screened regardless of family history.
Signs and Symptoms:
 Blood in or on the stool (either bright red or very dark in color)
Blood in or on the stool (either bright red or very dark in color)- A persistent change in normal bowel habits such as diarrhea, constipation or both, for no apparent reason
- Frequent or constant cramps if they last for more than a few days
- Stools that are narrower than usual
- General stomach discomfort (bloating, fullness and/or cramps)
- Frequent gas pains
- A strong and continuing need to move your bowels, but with little stool
- A feeling that the bowel does not empty completely
- Weight loss for no known reason
- Constant tiredness
Note: Many people diagnosed with CRC never had any symptoms or early warning signs. Above are the most common signs of CRC, but it is important to note that the symptoms are not unique to CRC - check with your doctor if you suspect a problem.
Risk Factors:
There is no "single cause" for developing CRC, but there some people who are considered to be at higher risk than the general population for CRC include:
- People with a family history of CRC. If you have a first degree relative (parent, sibling, aunt, uncle, grandparent) with CRC, you should get tested 10 years before his/her age of diagnosis. If he/she was diagnosed at 48, you should be tested when you are 38 years old.
- People who have already been diagnosed with polyps or early stage CRC.
- People who have inflammatory bowel disease (ulcerative colitis or Crohn's disease).
- People with a family history of inherited breast cancer, uterine or ovarian cancer.
- Middle-aged people, 45 years and over.
If you are at higher risk, you should talk to your doctor about being screened as soon as possible.
The possibility of a diagnosis of advanced CRC in patients in their 40s is not uncommon and CRC has been seen in patients in their 20s. If you are concerned, get screened - there is not a health advantage to inaction.
Colorectal Cancer Rates Rising in Younger Adults
Colorectal cancer (CRC) is the second leading cause of cancer death worldwide and in the US when combining men and women. Alarmingly, it’s now the top cause of cancer death in men under 50 and the second in women of the same age group. This shift shows CRC affecting people as early as their 30s and 40s—a trend researchers attribute to a mix of genetic and environmental factors. These may disrupt the gut microbiome (the genetic material of microorganisms in the intestines), altering the immune system and increasing CRC risk in younger adults.
Prevention Starts with Screening
CRC is largely preventable with regular screening, now recommended to begin at age 45 (previously 50) for those at average risk. Screening methods depend on your risk level:
Average Risk (Age 45+, No Symptoms or High-Risk Factors)
- Fecal Immunochemistry Test (FIT): Yearly
- Cologuard: Every 3 years
- Colonoscopy: Every 10 years
Note: A positive FIT or Cologuard result requires a follow-up colonoscopy.
Symptoms Present?
- Rectal bleeding
- Changes in bowel habits
- Persistent abdominal pain
- Unintentional weight loss
- Chronic diarrhea
Action: Colonoscopy recommended.
Personal History?
- Previous colon polyps or CRC
Action: Colonoscopy recommended.
High-Risk Factors?
- Family history of CRC or precancerous polyps in a first-degree relative before age 60
- Multiple first-degree relatives with CRC or polyps
- History of Ulcerative Colitis or Crohn’s disease
- Known inherited CRC syndrome (e.g., Lynch syndrome)
Action: Colonoscopy recommended before age 45, with timing based on family history.
Advances in Detection
AI-powered polyp detection systems are improving outcomes. Studies show endoscopists with high adenoma detection rates (ADR) during colonoscopies better protect against CRC. With AI assistance, ADR increases by 14.4%, and every 1% ADR boost lowers the risk of interval CRC (cancer between screenings) by 3%.
The Good News
- Screening Gap: 1 in 3 US adults still skips CRC screening.
- Coverage: All health plans cover CRC screenings 100%.
- Survival: Early detection offers a 90% survival rate.
*Talk to your primary doctor today to schedule your screening.
Bal Raj Bhandari, M.D.
